Are you at risk of rheumatoid arthritis? Know your risk.
Dr. Sharad Jain
This article is about Rheumatoid arthritis. Know whether you are at risk of rheumatoid arthritis.
Read More
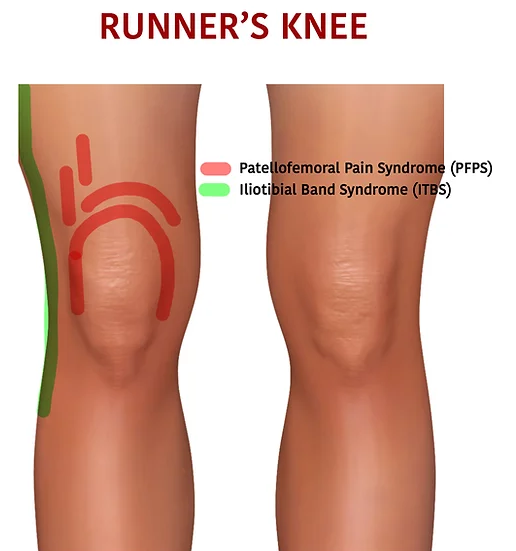
Patellofemoral Pain Syndrome (PFPS) involves pain around the kneecap's front, commonly known as
the patella—referred to as "runner's knee." Prevalent in runners and those engaging in running and jumping sports, the discomfort intensifies during activities like running,
stairs, sitting, and squatting.
Rest and ice aid milder cases, but physical therapy may be needed for severe instances. PFPS encompasses pain in the knee's front, particularly the patella, affecting
athletes and non-athletes alike. It hampers daily activities like stair climbing and kneeling. PFPS is frequent among athletes, especially runners and jumpers, but also
affects non-athletes, including adolescents, laborers, and older adults. It's the primary cause of knee pain, stemming from overuse, injury, or patellar misalignment.
The knee, the body's largest joint, is a complex structure composed of the lower femur
(thighbone), upper tibia (shinbone), and patella (kneecap). Ligaments and tendons form strong connections between the femur and lower leg bones, providing structural
integrity.
Muscles attach to bones via tendons, such as the quadriceps tendon linking front thigh muscles to the patella. Patellar retinacula, segments of this tendon, stabilize the
patella by connecting to the tibia. The patellar tendon bridges the patella and tibia.
Smooth joint movement relies on the interplay of structures. The patella resides within the trochlea, a groove atop the femur. Synovial fluid in the synovial joint minimizes friction, allowing the
patella to glide during knee flexion and extension.
Articular cartilage covers femoral ends, the trochlear groove, and the patellar underside, facilitating frictionless bone interaction. The synovium produces lubricating fluid, aiding motion.
A fat pad beneath the patella cushions and absorbs shock.
The patellofemoral joint, where the patella meets the femur, involves cartilage-covered sliding within the femoral groove. Collateral ligaments and synovial fluid enhance stability,
while bursae contribute fluid. The medial and lateral retinaculum patellar support patellar tendon attachment, maintaining knee integrity amidst intricate mechanics.
Overuse and Repetitive Activities: Running and jumping stress the knee joint, causing irritation beneath the kneecap, leading to discomfort.
Muscle Imbalances and Biomechanical Issues: Poor hip and knee muscle alignment can trigger patellofemoral pain, seen in inward knee movement during squatting.
Structural Abnormalities and Alignment Problems: Kneecap injuries or surgery increases the risk of patellofemoral pain syndrome, with trauma causing discomfort.
Age and Sex: Adolescents, young adults, and women due to pelvic anatomy disparities.
High-Impact Activities: Weight-bearing actions, like running, increase knee strain risk.
Foot Structure: Flat feet intensify knee pressure and susceptibility.
Mechanical Factors: Abnormalities such as hyperextension, torsion, or poor alignment impact kneecap function.
Biomechanical Factors: Weak hip abductors alter knee movement, possibly fostering patellofemoral pain.
Patellofemoral Pain Syndrome (PFPS) is characterized by a persistent, dull aching pain in the front of the knee. Exacerbated by activities like stair climbing, kneeling, and
prolonged sitting with bent knees, PFPS pain takes various forms. Individuals may experience discomfort during exercise, knee-bending activities, or after extended sitting.
Popping sensations when standing or ascending stairs are common. PFPS patients often report pain with specific movements:
Stair Movements: Ascending or descending stairs increases patellofemoral compressive forces, intensifying pain.
Sitting with Knees Bent: Prolonged sitting in a knee-flexed position aggravates discomfort.
Kneeling and Squatting: Activities involving knee flexion, like kneeling or squatting, exacerbate symptoms.
Diagnosis:
Diagnosing Patellofemoral Pain Syndrome (PFPS) involves thorough clinical evaluation and pertinent imaging tests. Patient history guides healthcare providers, who may perform physical
maneuvers and use imaging like X-rays, CT scans, MRIs, and ultrasounds to uncover potential causes. Physical exams encompass overall health, symptom duration, pain nature, and triggering
activities. Evaluation of knee stability, alignment, and range of motion, including squatting and jumping, aids in diagnosis. X-rays rule out bone damage, while MRIs offer insights into
soft tissue. This comprehensive approach ensures accurate identification of PFPS.
Differential Diagnosis:
Distinguishing PFPS from similar conditions is crucial for effective treatment. It's essential to differentiate PFPS from chondromalacia patellae, IT band friction syndrome, patellar
tendinitis, osteoarthritis, ACL tears, and referred pain. Careful assessment, based on distinct symptoms and imaging, aids in correctly identifying PFPS. This precise diagnostic process
enables healthcare providers to tailor treatment strategies to address the underlying condition accurately.
Conservative Treatment Approaches and Pain Management:
The management of Patellofemoral Pain Syndrome (PFPS) typically starts with non-invasive methods and pain relief strategies. Strengthening leg and hip muscles helps maintain knee stability,
while exercises guided by a physical therapist improve movement patterns. Weight loss can alleviate stress on the knees, and proper warm-up and stretching techniques reduce strain.
Over-the-counter pain relievers offer temporary relief. Physical therapy includes rehabilitation exercises, supportive braces, taping, and icing. Orthotics and knee-friendly activities
aid in the recovery process. Surgical intervention is considered only in severe cases.
Rehabilitation Strategies:
Physical therapy is a central component of PFPS management, involving tailored exercises to enhance muscle strength and knee alignment. Emphasizing quadriceps strength and core stability is crucial.
Orthotics and supportive braces may assist, while icing and taping could help alleviate pain. Surgical options, such as arthroscopy, debridement, lateral release, and tibial tubercle transfer,
are reserved for cases unresponsive to conservative measures. Prevention strategies encompass proper footwear, thorough warm-up, controlled training progression, and maintaining a healthy weight.
Holistic care aims to achieve pain relief, functional restoration, and the prevention of recurrences.
Patellofemoral Pain Syndrome (PFPS), often referred to as "runner's knee," involves discomfort around the front of the kneecap. It affects various individuals,
impacting daily activities such as climbing stairs and kneeling. Diagnosing PFPS necessitates a comprehensive approach, including patient history, physical examination, and imaging.
Conservative treatment methods, such as physical therapy, exercises, and pain relief strategies, are key in managing PFPS. Encouraging early intervention and a holistic approach is crucial
for effective treatment and preventing future occurrences of PFPS, allowing individuals to regain pain-free movement and optimize knee health.
We write the blogs time to time to guide website visitors about Symptoms, Causes and Treatments

Dr. Sharad Jain
This article is about Rheumatoid arthritis. Know whether you are at risk of rheumatoid arthritis.
Read More
Dr. Sharad Jain
A large number of people are effected by arthritis in Meerut. Read the article for details.
Read More